Antibiotic Resistance is Becoming a Major Threat to Humanity

As humans, we face a number of threats from the environment, but none may loom larger than the one posed by antibiotic resistance. Through our over prescription, poor regulation, agricultural abuse, and weak supply chains, a hyper-resistant bacteria is just around the corner. And unless we do something to change the tide, we may be looking at a pandemic of mass proportion.
Human presence on earth is a blip on the timeline compared to bacteria. And bacteria are pervasive; on our clothes, in our bodies, in dirt, and on the surface of pretty much everything – in fact, all of the bacteria on Earth, despite its microscopic size, would outweigh us 100 million times.
In the 3.5 billion years bacteria have lived on Earth, it has survived interminable challenges to its existence, which has only given it time to continuously adapt and outlast every other lifeform. Not to mention the fact that bacteria can reproduce 500,000 times faster than we can, with certain strains giving rise to a billion offspring within several hours.
Now that we’ve made it our mission to maintain sterile environments and avoid illness, we’ve been combating bacteria with chemicals and antibiotics every chance we get. Antimicrobials are used in everything from hand soap, to skin wipes, to yoga mats and kitchen towels, creating what can only be described as a Darwinian battleground, where only the strongest bacteria survive.
The Overuse of Antibiotics
Antibiotics were discovered during WWII, and prior to it’s discovery thousands of soldiers died from infection. When it became evident that antibiotics could easily cure bacterial disease, they became an instant panacea. But they weren’t used with a calculated strategy. Instead they were given as prophylactics, starting a dangerous trend of over-prescription.
Soon, the miracle drug known as penicillin was being prescribed by every doctor, whether there were only marginal chances an illness was caused by bacteria or not. And today that practice continues as doctors, who treat individuals, not society at large, would rather take the risk of over prescribing than having a patient get ill. It’s estimated that a third of all antibiotics are prescribed inappropriately, either when no bacterial infection is present, or the wrong antibiotic is recommended.
In 1945, the founder of penicillin, Alexander Fleming, warned the New York Times that doctors over prescribing the drug posed a serious threat to its efficacy. Though it wasn’t until the 70s that the FDA realized the potential fallout of antibiotic resistance.
By this point antibiotics were being used not just for humans, but almost universally for livestock as well. Farmers found they could raise animals in smaller, dirtier conditions if they staved off illness by incorporating antibiotics into their diet. And for some reason, still unknown to this day, a diet supplemented with antibiotics allows animals to grow slightly faster, producing more meat and subsequently more profit.
Today approximately 80 percent of all antibiotics in the U.S. are given to livestock, with the majority administered to healthy animals. This has created a vicious cycle in which farmers rely on the use of antibiotics to earn thin profit margins that would be eliminated if laws were enacted to restrict their use. Meanwhile, we’re eating the meat of these animals pumped with antibiotics, causing unknown health effects to us, while simultaneously promoting the growth of resistant bacterial strains.
Watch a trailer for the documentary, Resistance:
Antibiotic Resistance Causes: A Lack of Regulation
According to a 2016 World Economic Forum study, around 700,000 people die annually from antimicrobial resistance. That death toll will reach a total of 10 million by the year 2050.
So, why has the use of antibiotics been unregulated for so long? One answer is the rise in confinement agriculture, which put small farmers out of business and corporate agriculture at the forefront of meat production.
By the time the FDA realized the impending threat posed by antibiotic resistance and abuse, its widespread use was already ingrained in farming practices. The FDA proposed a ban for the use of antibiotics in animal feed by 1973, though it never came to fruition. Since then, the drug’s use has continually increased. The FDA merely provided recommendations to farmers to curtail the use of antibiotics, rather than getting legislation passed to mandate it.
So, who is preventing such legislation from being passed? Lobbyists from many industries, including big ag, pharmaceutical companies, and fast food chains relying on large quantities of cheap meat.
Today, there are nine billion animals raised for meat in the U.S. annually, with 90 percent of those animals raised in concentrated animal feeding operations, or CAFOs. These CAFOs, that contribute to a number of public health problems, are often owned by large corporations that pack as many animals into their enclosures as possible, barely maintaining their health with antibiotics.
Since the 1980s, mega-farms have overtaken markets, putting 85 percent of small farmers out of business. They began producing more meat at a faster rate, driving the market price of an animal down, sometimes by more than half. Now that this has become common practice, farmers fear they can’t afford to take a step back and revert to pre-antibiotic farming practices.

Misuse, Overuse and Refuse
The U.S. healthcare system is flawed, causing many to resort to desperate tactics when in need of medicine. While antibiotics aren’t necessarily expensive compared to other drugs, a trip to the doctor can cost the uninsured hundreds of dollars. To avoid this, people take matters into their own hands to save a buck, contributing to a greater problem and also putting them in a dangerous position.
On the extreme end, people have begun using over-the-counter animal antibiotics from pet stores to treat bacterial issues ranging from infections from wisdom teeth extraction to bronchitis. On the less extreme end, people often save unfinished antibiotics for future illness.
There’s debate as to whether patients should finish a prescription or stop once they start feeling better, but typically the dosage and type of antibiotic are tailored to a specific infection. There are also different strengths of antibiotics that have slowly become ineffective as bacteria have grown resistant. And not finishing a prescription can leave bacteria in your body that can grow stronger.
But even if we take proper dosages and get prescriptions from a doctor, there’s still the problem of waste and antibiotics seeping into the environment from a multitude of sources. Pharmaceutical pollution creates a fecund environment for antimicrobial resistance, and recent events have only perpetuated this.
A few years ago, there was an explosion at a Chinese factory that produced antibiotic precursors. This undoubtedly lead to more pollution, but it also lead to a major gap in the global antibiotic supply chain that relied on a tenuous supply of the drugs. This shortage, particularly of one antibiotic that prevents the spread of syphilis from mother to child, can exacerbate antimicrobial resistance while allowing the spread of disease.
Now that bacteria are evolving to quickly become drug resistant, pharmaceutical companies and their investors have no incentive to finance research into new antibiotics that could become useless within five years. When it costs a billion dollars to bring a new drug to market, there’s no chance our capitalist model will produce them at a loss.
What can we do before it’s too late? Awareness and pressure on the government to pass legislation limiting antibiotic use is key. While it seems hopeful at best, raising awareness can lead to a greater number of people observing best practices that limit resistance.
Pressuring governments, organizations, and private companies to enact policies can lead to change too. Encouraging doctors to prescribe fewer antibiotics, while consuming fewer ourselves, especially those from alternative sources, can slow the process of resistance.
Currently, one company, CARB-X, is working to speed up the development of new drugs that most big pharmaceutical companies won’t consider. The company’s funding is a mix of private and public partners working to find solutions to antimicrobial resistance.
In the E.U., the use of antibiotics in agriculture has been banned, and though there has been a slight decrease in animal growth and a slight increase in animal mortality, overall meat production is higher than when antibiotics were used.
If they can do it, so can the U.S. And though it may seem like something beyond individual control, it can be possible to collectively enact change by starting at the individual level.
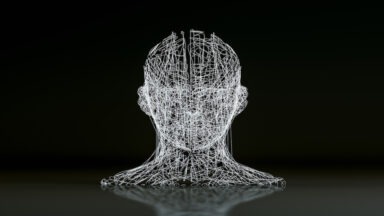
Should We Be Hesitant to Embrace Transhumanism?

The human body has somewhere in the vicinity of 50 to 100 trillion cells, depending on who you ask. Each of these cells has .07 volts of electrical energy potential — a relatively small number you might say. But when you multiply those .07 volts times 50 to 100 trillion, you get somewhere between two and a half, to five trillion volts. We are powerhouses of electrical energy potential.
Yet for some, this potential isn’t enough. In the minds of transhumanists, the body is a work in progress — one in which we must actively improve toward some perceived ideal. In some circumstances they may be right; our bodies are not all created equally, some face deformities and defects, or aren’t built as sturdy as others, making a good argument for the need to artificially augment.
But according to researcher and author Gregg Braden, this is a slippery slope — one in which we must tread with caution while appreciating the truly high-tech construction of the biological suits we’ve found ourselves born into.
“All of the technology that is now being developed in the world around us, and I worked in the Cold War years in the defense industry, space-based lasers, ‘Star Wars’ Defense Initiative… and I have yet to this moment, seen any tech in the world around us that does not mimic what we already do in our cells, except our cells do it better,” Braden said in a recent interview with Regina Meredith on Open Minds.
With advancements in microchip technology, futurists envision a world in which we begin to work toward almost complete integration with technology and computers. Some even go so far as to believe we will one day be capable of transferring our consciousness onto a hard drive composed of microscopic silicon chips, experiencing the world through that mechanistic, binary scope of the computer — potentially allowing humans to achieve something that looks like immortality.
But this reductionist mindset of the materialist, scientific lens is incredibly arrogant, Braden said.
Firstly, science’s “hard problem of consciousness” currently limits it from understanding what exactly consciousness is and where it comes from. And secondly, would this really even be the same kind of consciousness? Can you separate consciousness from our biological nature? And if you could, why would you?
Those are the two trains of thought when it comes to the views of our advancing technology and the transhumanist movement, Braden said.
One side views it as, “If we were never supposed to learn how to achieve such a feat, why have we gotten this far?”
While the other side says, “Just because we can, doesn’t mean we should.”