Gut Bacteria May Be Controlling Your Mood, Should You Fix It?
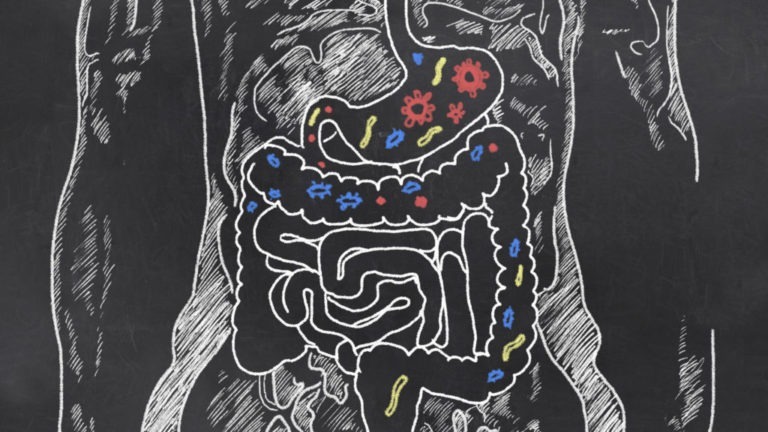
A unique force inside of us controls our bodies, emotions, and thoughts. It’s not our soul, mind, or sense of free will; it’s the microbes living in and on our bodies, outnumbering our cells by tenfold. In fact, there are 100 trillion of them, and those inside our gut have been found to influence and control our mood and behavior.
Gut Bacteria and Mood
The living culture of bacteria in our gastrointestinal tract, known as the gut microbiome or microbiota, consists of four pounds of biomass and is part of the 3 percent of our body weight that is made of microbes. While a third of that microbiome is consistent in all humans, the rest is unique to each individual.
The residual effects of our gut health can be as profound as changing the function of our brains. It turns out that the old axiom of going with your gut feeling is not just a colloquialism; it actually has some scientific basis.
Researchers have discovered the diversity of healthy gut bacteria in our microbiome often fluctuates and changes based on what we consume or the lack thereof. So, the choices we make in deciding what to put in our bodies can have a drastic effect on the makeup and health of our gut.
When our bodies don’t receive the nutrients they need, the microbes in our gut send metabolites through the enteric nervous system, or ENS, a multi-layer lining in our intestinal tract composed of hundreds of millions of neurons connected to the brain. Scientists think the vagus nerve is the pathway between the brain and the ENS, and is responsible for telling the brain what the body needs.
It can also tell the brain how to behave.
There’s a reason why certain foods change your mood or make you feel a certain way. Fatty acids in particular are detected by cell receptors in the brain and make up a significant portion of the its weight. This is why Omega-3s are known to be mental boosters, as the brain relies on them to balance mood, energy, and memory.
Certain neurotransmitters that regulate these brain functions are produced in the gut. In fact, roughly 90 percent of serotonin is produced in the gut.
Gut Health and Depression
Researchers conducted a test on mice to see if specific character traits like anxiety or depression had anything to do with gut bacteria. They found that mice exposed to specific gut bacteria, compared to those kept sterile, showed symptoms of anxiety and depression after being exposed to stress early in life. The sterile mice did not show these symptoms until they were also exposed to that gut bacteria.
Although both groups originally showed a release in the stress hormone, corticosterone, it wasn’t until the gut bacteria was introduced to the sterile group that they showed signs of depression. This test effectively demonstrated the symbiotic relationship between the gut and the brain and how it can have definitive effects on our mood and emotion.
In fact, some researchers are working on what they’re calling psychobiotics, medicine that targets mental disorders through the gut microbiome. Traditionally, it has been thought that gut-related illnesses, like irritable bowel syndrome, were caused by depression, stress, and anxiety, but now some researchers are starting to think it’s the other way around.

How to Restore Gut Flora
The myriad microbes in our gut, often referred to as our gut flora, thrive when fed properly. A study of a primitive tribe in Tanzania, known as the Hadza tribe, found a significant variation between their gut flora and ours. This tribe, specifically a smaller sect of them who were hunter-gatherers, maintained a diversity of berries, fruit, starch, and meat in its diet.
These people also consumed high levels of fiber – ten times more than the average western diet. In one day, this tribespeople would consume 100-150 grams of fiber. While this may sound like a copious amount, it seems this tribe has figured out the right gut-health diet. Scientists found this diversity to be essential in maintaining diverse gut flora and the key to feeding a healthy microbiome.
In addition to the lack of fiber consumed in Western diets, we consume a lot of refined sugar and processed food. Unsurprisingly, this destroys certain gut flora that is so essential to a good bacterial balance.
There are ways for rebalancing gut bacteria, namely through probiotics. Any naturally fermented or cultured food is good for promoting healthy gut bacteria. The probiotics that are best for improving gut flora are those that promote the growth of Lactobacillus. This strain of bacteria is often found in yogurts, cheese, and pickled foods. There is even research underway to develop a probiotic beer, as Lactobacillus has become the main bacteria used in sour beer.

Antibiotics and Gut Flora
It’s not just our diets that can have a serious impact on our gut health. By nature, antibiotics kill bacteria in our body including gut bacteria, and they do so indiscriminately. While antibiotics have been incredibly beneficial in preventing some deaths and illnesses, the extent to which we use them has created many negative side effects, especially when it comes to a healthy gut balance. Studies have found that it can take months for our gut microbiome to recover from the effects of antibiotics, and in some cases, up to a year.
While a healthy adult might be more concerned with catching an antibiotic-resistant pathogen than suffering from temporary gut flora damage, infants and young children are most susceptible to long-term effects. Scientists believe the administration of antibiotics in infants can lead to an imbalanced microbiome, impeding nutrient absorption, and immune system functions.
Some doctors even believe that children might develop autism due to damaged gut flora. This could also be related to children who develop ADHD, ADD, OCD, dyslexia, and dyspraxia. Although this is an incredibly contentious topic, more and more scientists are finding that gut flora is important in early development. Could there be a correlation between the decline in gut flora diversity in our Western diet and an influx of certain developmental issues in children? Will the gut be the next area of focus for treating mental diseases and disorders?
Gaia's Top 10 Videos on Holistic Health and Lifestyle

How do you discover your own path of well-being and vitality to achieve optimal health? The road is different for everyone and is an enduring, life-long mission. We invite you to sit with experts, from various health-related fields, who share the fruits of their research on nutrition, supplements, dentistry, detoxing, and unlocking our full health potential. What you may discover could change every aspect of your life.
1. The Gut Movie
In The Gut Movie, we follow the journey of journalist and researcher Kale Brock as, in the quest to discover whether the “optimal microbiome” does indeed exist, he travels from Australia to Namibia to live with The San, an ancient hunter-gatherer people living traditionally from the land. During the excursion, Brock monitors his own microbiome and how it changes in conjunction with the new surroundings and takes microbiome samples of The San to gauge the significant differences in microbiota present across cultures.
With expert commentary by leading gastroenterologist Professor Thomas Borody, molecular geneticist Dr. Margie Smith, immunology researcher and expert Professor Mimi Tang, naturopath and chiropractor Dr. Damian Kristof and others, The Gut Movie provides an insightful yet entertaining look at the explosive research of the gut and its impact on human health.